Chapter 5 – Gastrointestinal System Assessment
Abdomen – Auscultation
Auscultation of the abdomen as it relates to the GI system is performed to assess for intestinal function, specifically bowel sounds. Bowel sounds are produced by the movement of fluid, gas, and contents through the intestines.
As a nurse, auscultating for bowel sounds with the stethoscope’s diaphragm is a common part of health assessment. The diaphragm is best for detecting high-pitched sounds such as bowel sounds. Bowel sounds are sometimes loud enough to hear without a stethoscope.
Auscultation of the abdomen follows inspection, so the abdomen is already exposed. When conducting auscultation, begin in the right lower quadrant and progress clockwise to the right upper quadrant, left upper quadrant, and the left lower quadrant. Figure 5.5 presents the pattern of auscultation. Always begin in the right lower quadrant because this is the location of the ileocecal valve, which is a muscular sphincter that allows contents to move from the ileum of the small intestine to the cecum of the large intestine.
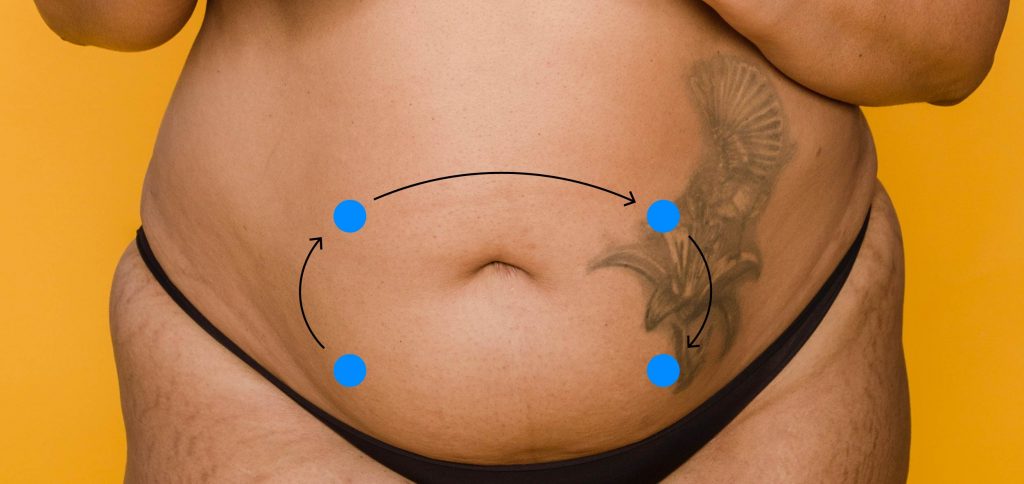
Figure 5.5: Pattern of auscultation.
Assess the presence, frequency, and quality of bowel sounds.
- Presence. Normally, bowel sounds are present in all four quadrants. This means that peristalsis is occurring and contents are moving through the intestines. Only document the absence of bowel sounds after listening in each quadrant for five minutes. Absent bowel sounds are a cue that suggest there may be a problem with the movement of contents through the intestines: common causes include , a complete bowel obstruction, or perforation of the small or large intestine. However, keep in mind that movements of contents and contraction of the intestines do not always create sound.
- Frequency. If you hear bowel sounds, describe the frequency (i.e., the rate of occurrence, how often do you hear them). You do not need to count the number of bowel sounds; instead, estimate whether they are considered normoactive, hypoactive, or hyperactive.
- Normoactive: 5–30 bowel sounds per minute (about 2 sounds every 5 seconds). Generally, you will only need to listen for a few seconds to estimate this frequency.
- Hypoactive: less than 5 bowel sounds per minute. Because the frequency of hypoactive sounds is less frequent, you will need to listen a bit longer in order to assess them. These sounds indicate that intestinal activity has slowed, which is normal when a person is sleeping. Hypoactive bowel sounds should act as a cue in other situations, which should always be assessed further. For example, bowel sounds may become hypoactive post-surgery due to anesthetic use and with certain medications (e.g., narcotics). Constipation is also a common cause of hypoactive bowel sounds.
- Hyperactive: more than 30 bowel sounds per minute. Again, you will only need to listen for a couple seconds in order to estimate this frequency. These sounds indicate that intestinal activity is quicker than normal. You will often hear hyperactive bowel sounds after a client has just eaten; these sounds may also be associated with diarrhea and early/partial intestinal obstruction.
- Quality. Describe the quality of the bowel sounds (e.g., the description, how they sound). You might describe the quality as high-pitched with a series or mixture of sounds (e.g., gurgling, rumbling, bubbling, and even clicking). You might describe the quality of sounds as irregular (i.e., no specific/constant rhythm). The quality of bowel sounds is typically less important than the presence and frequency, but an extremely high-pitched bowel sound can be a cue suggestive of an early bowel obstruction.
Auscultating the abdomen for bowel sounds involves the following steps (see Video 5.2):
1. Cleanse the stethoscope.
2. With a complete seal and light touch, place the diaphragm of the stethoscope on the abdomen in the right lower quadrant and listen. Next, lift the diaphragm and place it in the next quadrant.
3. Identify the presence and location of bowel sounds.
- Normally, bowel sounds should be present and heard in all four quadrants.
4. Identify the approximate frequency of bowel sounds. You do not need to count them.
5. Identify the quality of bowel sounds.
6. Note the findings.
- Normal findings might be documented as: “Normoactive bowel sounds heard in all four quadrants. High-pitched, gurgling sounds.”
- Abnormal findings might be documented as: “Hypoactive bowels sounds in all four quadrants.”
Video 5.2: Auscultating the abdomen
Priorities of Care
Any abnormal bowel sounds should be investigated. They should not be evaluated in isolation: an abnormal sound should always be considered in the context of other symptoms such as abdominal distention, flatus, pain, nausea, vomiting, diarrhea, and constipation. If a client has absent bowel sounds, consider whether this could be associated with a complete bowel obstruction, a perforation of the small or large intestine, or . All of these issues require urgent intervention and are often associated with pain, abdominal distention, nausea, and vomiting. If you suspect one of these conditions, monitor the client closely while conducting a primary survey and complete set of vital signs. Then, notify the physician or nurse practitioner.
Normal bowel sounds are usually the same throughout all four quadrants, but abnormal bowel sounds can vary from quadrant to quadrant. For example, hyperactive bowel sounds can be present prior to the location of a partial bowel obstruction, and hypoactive or absent after the location of a partial bowel obstruction. Trends in bowel sound are important to consider; for example, a sudden shift from hyperactive to absent may indicate a crisis situation such as a bowel perforation.
Activity: Check Your Understanding
refers to inflammation of the peritoneal cavity that can be caused by a variety of conditions.